Key Takeaways:
- Unfilled roles create hidden costs that ripple across safety, morale, and revenue.
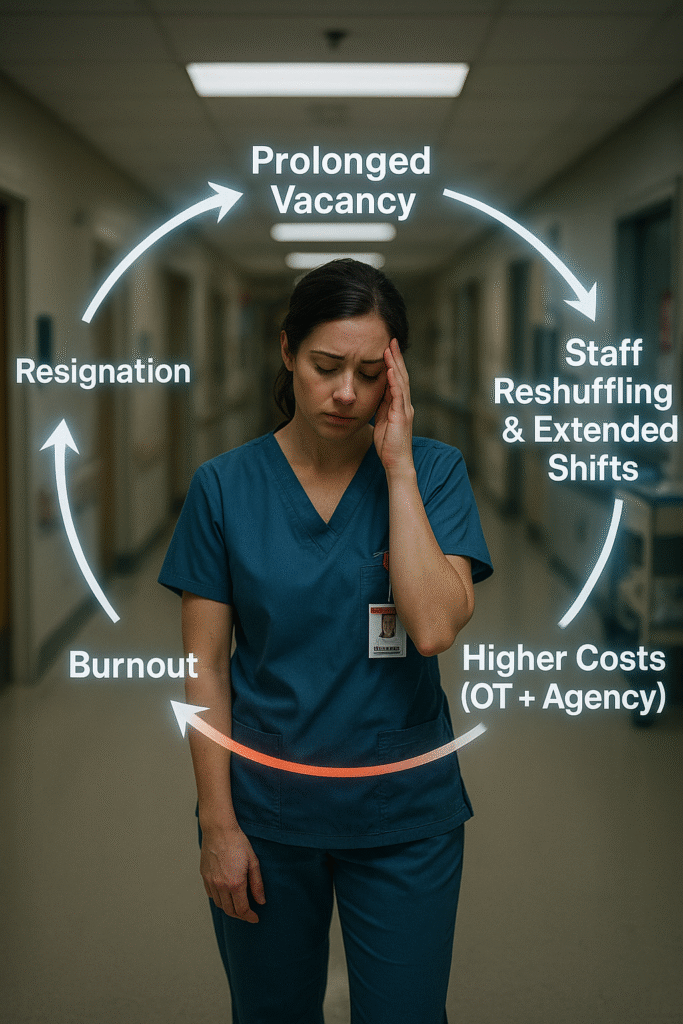
- The “backfill spiral” transforms staffing gaps into long-term dysfunction.
- Hiring delays lead to quantifiable losses in liability, turnover, overtime, income, and reputation.
- Recruitment must be treated as a strategic lever, not a back-office function, to restore operational and financial health.
By Tiny Manyonga
Replacing one registered nurse can cost up to $64,000 – more than eight months of salary per RN lost. Yet many health systems still treat recruitment as a background task, managed reactively, and funded begrudgingly. The result? Staffing shortfalls that quietly bleed hundreds of thousands, far more than the cost of any job post.
For hospitals and care networks, the most expensive staffing decisions are not the ones that are made; they are the ones delayed. Reactive recruitment, still a favorite healthcare staffing strategy across much of the industry, is the hiring equivalent of the hospital pager: familiar but dangerously obsolete. While recruiters wait for job requisitions, managers scramble to reshuffle teams, stretching staff until something breaks. This is Code Blue hiring, crisis-mode staffing that only kicks in when the damage can no longer be ignored. It is outdated, expensive, and clinically dangerous. It is not intentional, but it is inevitable, given how most systems are built.
Beyond leaving coverage gaps, vacancies trigger a chain reaction known as the backfill spiral. When one nurse leaves, the initial strain feels manageable. But then coverage shifts, overtime piles up, and those picking up the slack burn out or leave themselves. That departure restarts the cycle.
Let’s Talk Real Money
Reactive hiring quietly masks these downstream effects. When a position is finally filled, leadership often moves on. However, the damage accumulates in ways that do not show up on spreadsheets: onboarding shortcuts, training delays, and a compromised safety culture. Back-to-back temporary coverage may have kept shifts going, but it often deepens churn rather than resolving it. Before building better pipelines, leaders need to recognize that delays are not neutral. They are deeply expensive liabilities that compound over time.
Beyond being a scheduling problem, staffing shortages are a clinical and financial hazard. Understaffed units lead to overworked nurses, who are more likely to make medication errors, miss critical handoffs, or suffer communication breakdowns. The result? Over 7 million patients in the US are harmed by medication errors, costing at least $40 billion annually in healthcare expenditure – half of that ($21 million) represents preventable errors. From the perspective of healthcare facilities, an actuarial study estimated that preventable adverse events result in $17 billion in extra costs incurred by providers.
These are considerably large macro-level costs that may be difficult to translate to consequences on an organization’s bottom line, yet they do impact individual facilities. A single adverse event can add nearly $59,000 in extra treatment costs. If negligence is involved, that figure climbs above $110,000. Preventable medication errors, often the result of fatigue and short-staffing, add an average of $2,200 to $4,600 per incident, primarily from extended hospital stays. And communication breakdowns, a predictable outcome when teams are stretched thin, drive malpractice claims averaging $237,000 per case. Even one missed handoff or misunderstood instruction can trigger six-figure liability. This does not even consider the costs associated with replacing an RN.
Understaffing is a double-edged sword that drives up clinical errors while accelerating staff attrition. Burned-out and overworked nurses tend to leave, and the replacement costs are significant. These include separation, hiring, and training costs, and they average at least $56,000 per bedside RN.
For a small facility with just twenty-five nurses, considering the average 22.5% annual turnover, replacing nurses can cost between $264,000 and $336,000 just in direct expenses. It does not account for overtime, temporary staff, or the downstream clinical impact of understaffing during transitions. Furthermore, Oracle’s healthcare labor study reports that replacing a regular position costs between 6 – 9 months of the employee’s salary, but a highly specialized healthcare professional can cost as much as double their annual wage.
To plug in the gaps, many facilities turn to overtime and agency nurses. As expected, overreliance on overtime exacerbates the problem by increasing working hours and burnout. However, like agency or travel nurses, overtime inflates the wage budget. Overtime pay alone inflates labor costs by 50% or more, since federal law mandates time-and-a-half for any hours beyond 40 per week. On the other hand, stopgap agency hires carry anywhere between 20–65% markup over standard compensation, depending on the skills and experience required. Both options are unsustainable in the long run for both the facilities and their patients.
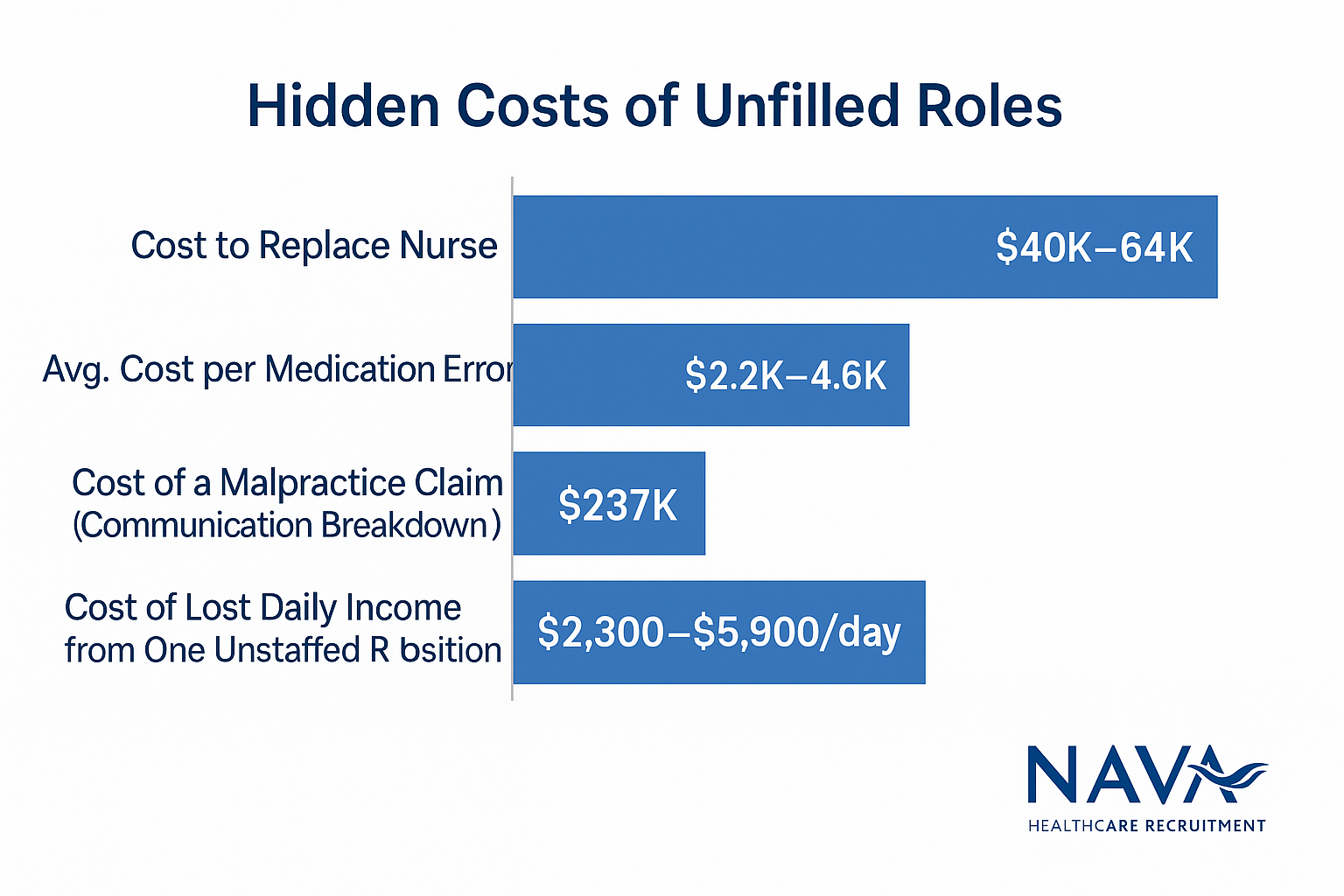
In addition to raising labor costs and potential liabilities, understaffing also suppresses income. Hospitals and care facilities across the U.S. have lost billions in revenue because they could not operate at full capacity. When facilities cannot admit patients due to a lack of staff, every empty bed represents lost daily income. Considering a RN can be assigned a maximum of 4 – 8 patients, depending on the facility, a vacancy costs regular facilities between $2,300 and $5,900 per day, depending on the region. It is likely higher in specialized facilities. Even in outpatient settings, backlogged clinics and provider staffing shortages have reduced throughput and daily visit volume, cutting into core revenue streams. Simply put, every unstaffed position is an unbilled service.
Lastly, revenue lost is not always directly measurable. The impact of understaffing ripples far beyond today’s balance sheet. When delays grow, safety incidents rise, and frontline staff are stretched too thin to deliver quality care, patients notice and never return. They may also have a thing or two to say on review sites, such as Glassdoor.
Declining satisfaction scores and word-of-mouth fallout lead to fewer referrals, reduced patient volumes, and penalties from payers. Under Medicare’s Value-Based Purchasing program, even a modest drop in HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores can cost a hospital up to 2% of its total Medicare revenue. That may not sound like much until you realize it can translate into millions in annual losses. In a market where every patient encounter is a revenue opportunity, reputational damage has a real, measurable cost.
Understaffing is not just bad math. It is a feedback loop of dysfunction: burnout, turnover, higher costs, lost income, and worse outcomes.
Transforming Your Favorite Healthcare Staffing Approach to a Strategic Lever
Most healthcare facilities do not neglect recruitment because they are indifferent. Rather, it is because they underestimate what lazy recruitment is costing them. Turnover gets written off as churn, and overtime becomes standard. But, by the time understaffing hits the balance sheet, it has already taken a toll through safety incidents, lost revenue, and legal exposure. That makes reactive hiring more than an operational flaw. It is a systemic liability, and the only way to contain it is by treating recruitment as a strategic lever.
Strategic hiring is not about faster fill rates. It is about changing the trajectory of your labor expenditure. That means building pipelines before vacancies hit, aligning talent with patient acuity, and treating retention not as a benefit but as a design principle.
Here is what that looks like in practice:
- Workforce planning integrated into budget cycles, not triggered by crisis.
- Exit and stay interviews informing staffing models, not just HR policy tweaks.
- Talent pipelines filtered for clinical compatibility and team cohesion, not just license status.
- Cross-functional partnerships across HR, clinical leadership, and finance to forecast needs before gaps emerge.
Forward-thinking systems are shifting from transactional hiring to long-term workforce strategies. And that’s where Nava Healthcare fits in.
Instead of chasing job board applicants or temp agency markups, Nava builds precision-aligned hiring pipelines tailored to each facility’s pace, culture, and care profile. We do not just source candidates, we stay connected with them. By maintaining active relationships with our talent pool, we ensure a pipeline of engaged, well-matched professionals who are ready when you are.
Our process reduces the financial bleed from misaligned hires by vetting for behavioral fit, not just credentials. We reduce agency expenditure by proactively maintaining talent readiness, not just scrambling to fill roles. And because we factor retention into recruitment, our placements stick, saving tens of thousands per head on retraining and backfill costs.
What Comes Next and Why It Matters
Understanding the full cost of reactive hiring and why it should not be your favorite healthcare staffing strategy is not the endpoint. It is the bare minimum.
While every executive and decision-maker reading this may accept that healthcare staffing is flawed, most have not calculated how deeply the damage runs. This is the moment to stop treating hiring like a support function. It is a financial risk and a clinical vulnerability. A systems problem that demands leadership-level solutions.
And this is just the beginning.
In the next article, we will show why slow hiring is not an accident but baked into healthcare hiring infrastructure. Then we will examine why the platforms recruiters rely on to find talent are quietly undercutting your efforts. We will reframe so-called “staffing shortages” as evidence of structural mismatch, and we will explore how burnout is not just a floor problem. Instead, it reflects upstream decisions that only the C-suite can fix.
From there, we will dig into the mechanics: requisition systems that block your best candidates, tech that overpromises and underdelivers, and what future-ready hiring really looks like when built to scale. If the failure is structural, the solution must be, too.
You do not need more vendors. You need a new framework and a partner who sees the whole board.
The question now is not whether you act. It is who helps you get there.