Key Takeaways
- Transactional Recruiting Fails: The standard healthcare staffing and recruiting agency model, which only matches technical keywords on a resume, is structurally blind to “soft skills” and is a primary cause of poor-fit hires.
- Compassion is a Core Competency: Emotional intelligence and empathy are critical, measurable business competencies that directly drive patient outcomes, staff retention, and financial performance.
- The High Cost of Poor Fit: A technically skilled but behaviorally misaligned hire directly erodes HCAHPS scores, impacts financial reimbursements, and increases malpractice risk.
- Internal Team Destabilization: A clinician with incompatible emotional intelligence creates team friction, undermines psychological safety, and accelerates burnout in their colleagues.
- The Relational Solution: A relational framework uses genuine rapport, not just tests, as the primary vetting tool to assess a candidate’s true emotional intelligence and cultural fit.
By Tiny Manyonga
Senior healthcare leaders are facing a polycrisis: persistent staff burnout, clinician turnover in a talent-scarce market, and declining patient satisfaction. With internal teams unable to keep up with the persistent need for qualified clinicians, healthcare facilities increasingly rely on recruitment agencies. However, many agencies in healthcare staffing and recruiting approach this as a simple volume problem, focusing on filling roles quickly with technically qualified candidates.
While this “transactional” model does result in positions filled, retaining clinicians remains a challenge. This is because simply throwing clinicians that tick all the boxes into the gaps is a strategy that fundamentally misunderstands the problem, mistaking a technically licensed clinician for a culturally and behaviorally aligned one. The research now overwhelmingly shows that “soft skills” like empathy and emotional intelligence are not “nice-to-haves”; they are core competencies that directly drive patient outcomes, staff retention, and overall financial performance.
There is a definitive business case for going beyond the usual metrics when selecting a recruitment partner and focusing on the “Compassion ROI.” The standard transactional vetting model is structurally blind to these critical soft-skills, and the costs of this disregard are both quantifiable and consequential. This analysis will quantify the high price of this systemic failure before presenting a “relational framework,” built on genuine rapport, as the only effective way to vet for and secure the patient-centered talent that truly defines a high-reliability organization.
The Transactional Model: Why Resumes & Checklists Fail to Measure Empathy
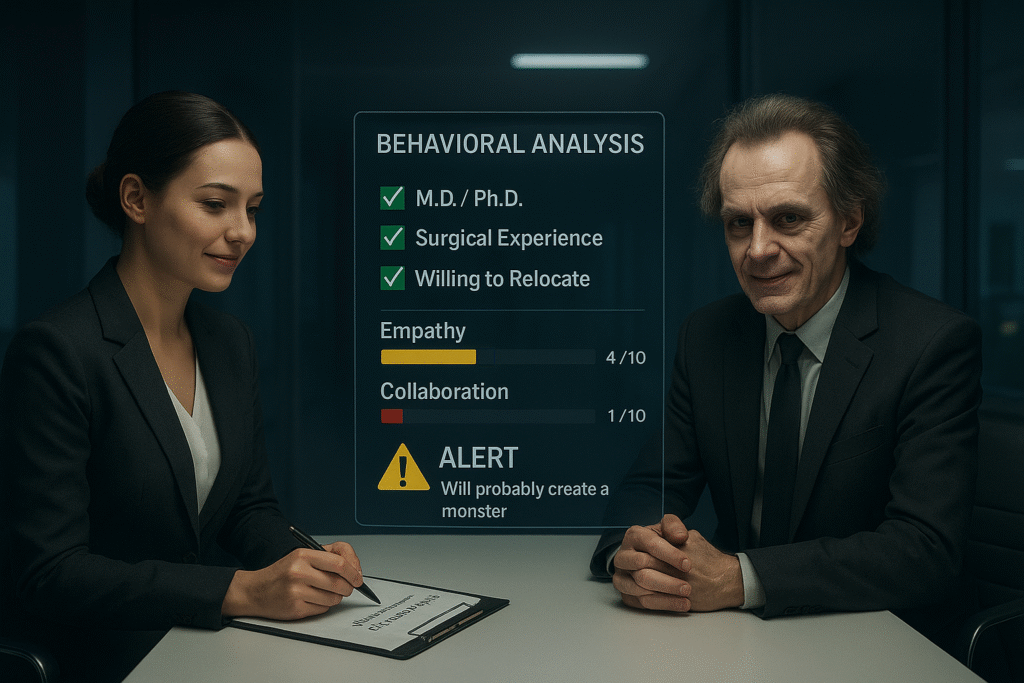
The standard agency model in healthcare staffing and recruiting is “transactional“; it is designed to match a resume’s keywords to a job description’s technical requirements. This process is structurally incapable of measuring, or even identifying, the “patient-centered” relational skills that are the true predictors of success at the bedside. This failure to vet for anything beyond a technical checklist is not a minor oversight; it is a systemic flaw that leaves a critical gap in the hiring process.
From Buzzword to Business Imperative: Defining “Compassion”
For decades, “compassion” and “emotional intelligence” have been dismissed as unmeasurable buzzwords in the high-stakes, technical world of healthcare. However, the data now defines them as critical, measurable business competencies that are foundational to clinical excellence. These are not just abstract ideals; they are the fundamental building blocks of patient safety, satisfaction, and staff stability. We must move them from the realm of soft ideals to that of measurable, manageable, and strategically vital assets.
We can define these competencies with clinical precision. Emotional Intelligence (EQ) is the foundational internal skill: the clinician’s ability to perceive and manage their own stress, remain resilient, and collaborate effectively within a high-pressure team, as clinical studies consistently demonstrate. Empathy, as defined by research institutions, is the cognitive and affective skill of understanding a patient’s emotional state. But the critical, actionable competency is compassion — the skill that translates empathy into a behavioral response and motivates a clinician to act to alleviate suffering. It is this combination, EQ for resilience, empathy for understanding, and compassion for action, that determines not just the existence of but the quality and safety of a clinical interaction.
Why the “Transactional” Model Fails
The transactional model, used by most agencies in healthcare staffing and recruiting, is built to optimize for speed and volume. It asks a simple, binary set of questions: “Is this clinician licensed?” and “Do they have two years of ICU experience?” It is a checklist designed to find a technically qualified unit, a “warm body” to fill a slot. The entire process is a box-ticking exercise, matching keywords on a resume to a job description, and it stops there.
This is a critical distinction. The failure of the transactional model is not about simply failing to screen out “uncompassionate” clinicians. The more costly failure is its inability to understand context. Granted, the vast majority of clinicians are empathetic and compassionate individuals. Regardless, the external pressures of a high-acuity unit, specific team dynamics, or a difficult patient population can impact even the best clinician’s behavior. A person’s ‘compassion’ is not a fixed trait; it is an expression of their EQ in a specific environment. A clinician who thrives in a methodical, long-term care wing may be a poor fit for a chaotic, high-stress ER, not because they lack compassion, but because their EQ is unsuited to that specific environment.
This model fails because it is structurally blind to the metrics that matter. It fails to ask the critical questions that determine a candidate’s actual on-the-job success: “How does this clinician respond to a distressed or non-compliant patient?” “How do they handle interpersonal conflict with a colleague during a high-stress code?” “How do they self-regulate to manage the burnout that comes with the job?” This systemic failure to vet for anything beyond a technical resume check is a structural flaw that guarantees a poor, high-risk fit.
The High Cost of Poor Fit: How Incompatible Emotional Intelligence (EQ) Erodes HCAHPS Scores
The failure to measure empathy is not a “soft” problem; it has hard, catastrophic financial and operational consequences. The “agitation” caused by a transactional, poor-fit hire — a clinician who is technically skilled but behaviorally misaligned — is felt directly in the hospital’s most critical, board-level metrics. As extensive research shows, a “compassion gap” is a primary driver of patient dissatisfaction (HCAHPS), staff turnover, and direct legal risk.
The Direct Link Between Empathy and HCAHPS Scores
The research is no longer ambiguous: the single greatest driver of patient satisfaction and HCAHPS scores is the perceived empathy and communication skill of the clinical staff. Studies consistently show that a patient’s perception of care is more heavily influenced by the way they were treated; whether they felt heard, respected, and treated with dignity, rather than the technical outcome of that care. A technically flawless procedure that feels impersonal or dismissive will result in a low score.
A poor-fit, transactional hire, one who is technically proficient but emotionally disconnected, abrupt, or poor at communication, can single-handedly erode a unit’s HCAHPS scores. This has a direct and immediate financial impact, as these scores are increasingly and publicly tied to Medicare, Medicaid, and Value-Based Purchasing (VBP) reimbursements. A “soft skill” deficit is, therefore, a hard-dollar revenue problem that transactional vetting completely ignores.
The Hidden Cost: Malpractice Risk and Staff Burnout
The agitation extends far beyond survey scores. A “compassion gap” is a primary and well-documented driver of patient complaints and, ultimately, malpractice lawsuits. Industry data is clear: patients who feel “unheard,” “ignored,” or “disrespected” by their clinical team are far more likely to litigate, often regardless of the technical quality of the clinical outcome. Vetting for empathy is, therefore, a core risk-management strategy that protects the hospital’s bottom line and reputation.
Internally, a clinician with incompatible emotional intelligence (EQ) is a destabilizing force. They create team friction, undermine psychological safety, and accelerate burnout in their colleagues by refusing to collaborate or creating a toxic environment. This directly impacts nurse retention, as high-performing staff will not tolerate a toxic or uncooperative team. This creates a costly turnover spiral that is rooted not in a lack of technical skill, but in a single, poor behavioral fit.
The “Rapport” Solution: A Relational Framework for Vetting Patient-Centered Talent
The only way to find true “patient-centered talent” is to abandon the transactional model in healthcare staffing and recruiting for a “relational” one. This requires a strategic partner who understands that a resume is data, but a person is a human. This “relational framework“ uses rapport-building as a core vetting tool, shifting the goal from “filling a slot” to making a genuine, holistic, human-to-human connection.
The “Rapport-Building” Differentiator
A transactional recruiter conducts an interrogation — a rapid-fire checklist of skills, experiences, and salary expectations designed to get a “yes” or “no” as fast as possible. A relational recruiter, by contrast, builds rapport. This is not just a stylistic preference; it is a fundamental strategic differentiator designed to elicit truth. This human-centered approach is a core component of the Nava Healthcare model.
By building a foundation of genuine human rapport, the recruiter creates a space for honesty and psychological safety. This is the only way to get past the canned “interview answers” and truly assess a clinician’s communication style, their resilience to burnout, and their core motivations. It’s how you discover why they are a clinician, not just that they are one. This reveals the very “emotional intelligence” (EQ) metrics the transactional model is structurally blind to.
Why True Rapport is Superior to Any “Test”
This “rapport-driven” model is not just a prelude to a test; it is the validation. The transactional model operates on a spectrum of such tests. At the low end, agencies rely on generic behavioral interviewing or hypothetical questions. More-sophisticated agencies, attempting to get better data, use advanced assessment tools like the Sinclair Compassion Questionnaire (SCQ) or the Schwartz Center Compassionate Care Scale (SCCCS). But while these advanced tests are more sophisticated, they still operate on the same flawed, transactional premise: forcing a candidate to give a “correct” answer in a high-stakes, one-hour window. This provides a single “transactional” data-point, not a true insight into a person’s character or resilience.
The Nava Healthcare relational model is fundamentally different. We build genuine, long-term relationships before a role is even on the table. This rapport is what allows our recruiters to get beyond “interview answers” and understand the whole person — their career goals, their personal challenges, and their core motivations. This human-centric data, gathered through trust, is infinitely more predictive of cultural fit and compassion than any standardized questionnaire.
Conclusion
For decades, healthcare staffing and recruiting has been treated as a commodity transaction, and the industry is now paying the price in the form of low HCAHPS scores, clinician retention problems, and endemic burnout. The problem is clear: resumes and checklists cannot measure empathy. They are the wrong tools for the job, and they are-failing to find the “patient-centered talent” hospitals need to thrive.
The only way to find these clinicians is to adopt a relational model. This model, as championed by Nava Healthcare, uses rapport-building as a strategic tool to open an honest dialogue, allowing for a true assessment of EQ. This is the “Compassion ROI”: an engineered solution that links a “compassionate,” clinician-centric vetting process directly to higher patient satisfaction, reduced legal risk, and a more stable, resilient workforce.
If your hospital or medical facility is ready to move beyond the high-risk, low-retention transactional model pervasive in healthcare staffing and recruiting, the next step is a strategic review. Contact Nava Healthcare to diagnose your current vetting process, eliminate structural blind spots, and build a relational framework engineered for retention and clinical excellence.