Key Takeaways
- Most healthcare staffing systems fail not from lack of insight, but from outdated infrastructure and strategic inertia.
- Tools like job boards and ATSs create noise without strategy. They can only support hiring strategy, but do not replace it.
- Transformation stalls because leaders fear mid-transition failure, yet inaction quietly sustains burnout and operational risk.
- Strategic hiring requires three pillars: proactive workforce planning, precision role design, and cross-functional execution infrastructure.
By Tiny Manyonga
Medical Recruitment is not failing for lack of analysis. We have dissected this problem from every angle: financial, operational, and technological. Healthcare leaders are not short on insight , rather they are disincentivized from building systems that hold.
This is the turning point in the series: from diagnosis to design, and from breakdowns to bridges.
A single RN vacancy can bleed up to $64,000 in replacement costs alone, but that is just the start. One empty role often triggers a backfill spiral that spreads burnout, damages care quality, and slashes revenue. We realized staffing shortfalls strain operations and quietly rack up millions in overtime, onboarding waste, and liability risk. All this culminates in plummeting patient satisfaction – which is not innocuous when, in fact, under Medicare’s Value-Based Purchasing program, even a minor drop in satisfaction scores can cost hospitals up to 2% of their total Medicare revenue.
The hiring delays are not merely unfortunate but engineered. Most hiring systems still run on legacy workflows built in an era of a surplus of skilled clinicians. We built intricate approval chains, created credentialing lags, and siloed ownership that all but guarantees missed opportunities. While healthcare delivery runs on clinical urgency, hiring operates like a bureaucracy – one where mutual ghosting is so common that over half of candidates drop out due to silence or delay.
By the time a healthcare facility has finished the paperwork and is ready to welcome a recruit, their preferred candidate is long gone. Then it is back to the backfill spiral: exhausted teams, fractured trust, and a growing sense that leadership simply is not moving fast enough.
So many have turned to “modern tools” for salvation.
Job boards, AI screeners, and ATS upgrades. Not bad concepts in themselves but are often miscast as strategy. These tools were built to support a strategy, not substitute for one. They deliver resumes, not readiness, and activity, not alignment. When leaders mistake tools for transformation, recruiters end up drowning in volume with no structure to sort signal from noise. The tools work, but only inside a system and strategy that does too. A system with the reach to surface the right candidates, the insight to assess fit beyond the resume, and the continuity to build pipelines that extend beyond organizational walls.
“We’ll Burn That Bridge When We Come to It”
We have identified and discussed a significant chasm between a well-functioning and strategic medical staffing strategy and the outdated systems in use. Executives are not ignoring the gap; they are staring right into the void. Every day brings another spreadsheet showing inflated overtime, another manager flagging a backfill spiral, and, perhaps, another resignation from a clinician who waited too long for reinforcements. While some complaints, like overextended teams and waning morale, are quiet grumblings, others are loud: patient dissatisfaction, regulatory flags, coverage shortfalls.
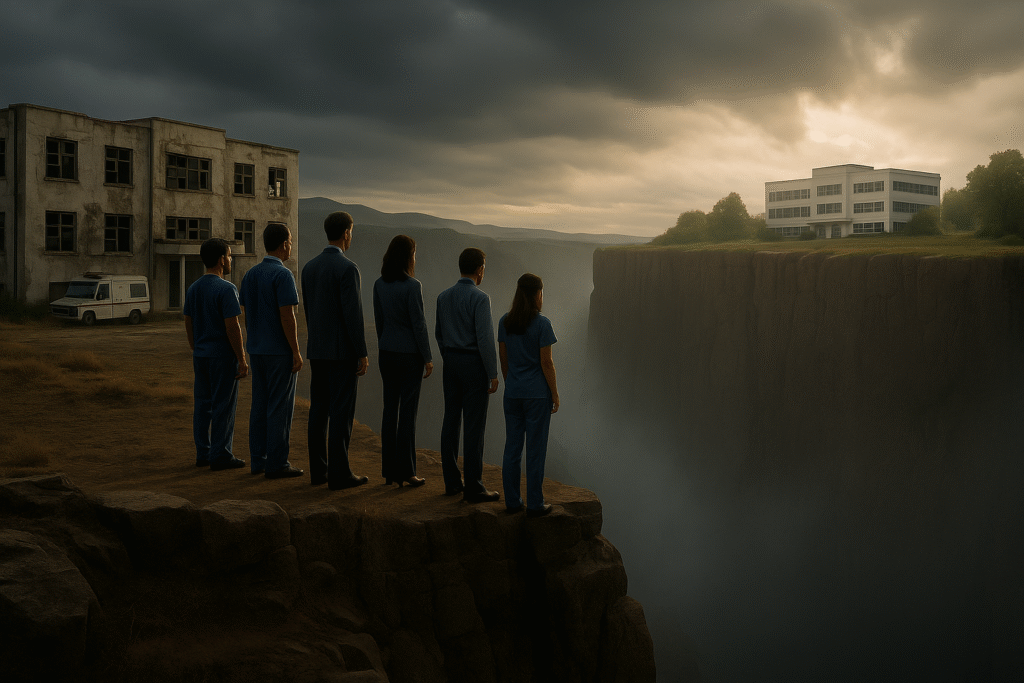
On the horizon, the promise of better recruitment and retention is real. Leaders can imagine a system that works; systems where the right talent arrives on time and pipelines stay warm, where hiring flexes with clinical demand. They can almost see it but, between that vision and the current reality, lies a leap of faith. A void filled with financial risk, clinical exposure, operational chaos, and reputational damage if the system buckles mid-transformation. Unsurprisingly, not many are queuing up to make the giant step forward.
That hesitation to take transformative steps on healthcare staffing is not just inertia, it is insurance. Behind every slow decision is a worst-case scenario: a department thrown into chaos mid-transition, a rushed hire who disrupts clinical culture, or even a delay in care traced back to a change not ready to be deployed. Reforming a workforce system is unlike flipping a switch. It impacts scheduling, billing, compliance, and continuity of care. One broken link can stall entire units, delay surgeries, or spark staff departures that, in turn, trigger even deeper coverage gaps. When executives hesitate, it is not because they do not care – it is because they know exactly how high the stakes are.
As such, they would rather wait, only to cross any bridge when the fires are closing in behind them and there is no other way around. The deeper challenge, the one that quietly locks these systems in place, is strategic inertia. It is the persistent belief that small tweaks will somehow yield transformation. From the outside, this may look like mere executive risk aversion in an industry and setting where failure is visible, consequential, and severely punishable. However, modernizing a healthcare recruitment system is not a remodel that merely requires the right tools; it needs an architect.
Designing Resilient Systems for Medical Recruitment
Strategic medical hiring is not a slogan. It is infrastructure: designed, aligned, and built to hold under pressure.
At the moment, most systems are not built for what they are facing. More than half of healthcare organizations still do not have a formal workforce plan, especially for contingent, behavioral health, or allied roles. Vacancies are chased after they open, pipelines stall, and short-term stopgaps disguise long-term dysfunction (Becker’s Hospital Review).
Strategic medical staffing is not just about “hiring faster.” It is about hiring differently, and that means building a system that is structurally capable of doing three things well:
- Talent Planning: This starts before the job is posted. Facilities must forecast needs based on clinical growth, population trends, and retirement risk. However, most cannot because workforce planning is reactive, not strategic. It’s driven by budgets and consequences, not demand (Advisory Board).
- Precision Role Design: One-size hiring fails fast. Each care environment demands its own sourcing strategy, hiring cadence, and cultural alignment. Regardless, most recruitment systems flatten these variables, which is why clinical leaders often reject candidates HR sends. They were not hired for and do not seem prepared or suitable the reality on the ground.
- Cross-functional Execution Infrastructure: Even the best plans can die in silos. Hiring spans HR, clinical, finance, and compliance departments but few systems align and coordinate those stakeholders. Decisions get lost in fragmented workflows, role recruitment stalls, and accountability diffuses. In the process, any momentum to urgently fill a necessary role evaporates, leaving clinicians to compensate for the gaps (McKinsey).
The result is a leadership paradox. As an executive, you may know what is needed to address the root causes. However, when your internal teams are already stretched thin, HR is burned out, clinical managers are firefighting, and finance is still attempting to trim costs, it is easy to miss the forest for the trees. No one has the time or perspective to architect a better system while managing the crisis of the current one (Health Affairs).
Most organizations that try to plan or redesign their workforce systems hit the same walls: lack of executive buy-in, budget limitations, and political risk. According to a 2023 national review of hiring systems, many leaders acknowledge the need for coordinated hiring strategies but find themselves unable to act without sacrificing short-term productivity or financial targets (Healthcare Workforce Recruitment – Challenges, Solutions, and Barriers (2022–2025)). Others are blocked by the absence of shared data infrastructure or struggle to coordinate across internal departments long siloed from one another.
Even promising attempts at reform are often undermined by the absence of a guiding system. When individual tools, AI screeners, pay bumps, new job boards, are deployed without strategy, they fail to resolve the underlying issue. In some cases, they exacerbate it. They present a larger pipeline with no clear screening method and faster approvals with no context on long-term fit. More applicants, fewer hires, and burnout on both sides of the table.
And so, the chasm stays looming while risk avoidance wins. And the cycle of burnout, churn, and misalignment continues.
From Collapse Risk to Lift-Off: Gain Altitude in Healthcare Hiring
Armed with these insights, any healthcare leader probably reaches the same conclusion: we must try; the system will not fix itself. So, they try to cross the chasm, one plank at a time, every initiative a makeshift beam, trying to bridge the gap. But when internal teams are locked in daily firefighting, they cannot architect the systems they need to carry the weight of the transformation. Even the most experienced CHRO cannot build a modern recruitment engine, not while requisitions pile up, urgent hires drain focus, and approvals stall.

Crossing a valley without full visibility, aligned infrastructure, or time to architect thoughtfully invites collapse. At the moment, healthcare leaders feel the pressure and need to the bridge while crossing it. Every initiative becomes an ad hoc column; disconnected, unstable, and often unsupported. But this chasm is not just wide; it is deep. Below lies clinical disruption, operational breakdown, and reputational fallout. In healthcare, a misstep mid-reform does not just slow progress, it breaks systems. Urgency alone will not carry you across. What you need is coordination, precision, and reach.
That is why some of the most forward-looking systems are shifting posture and not just outsourcing tasks but externalizing transformational risk. They are not trying to build a bridge mid-crossing. They are finding partners with the altitude to fly over the valley altogether.
Nava Healthcare Recruitment is not a vendor. We are a systems partner to healthcare leaders who understand that temporary fixes no longer hold. We design aligned pipelines with a focus beyond placing physicians, nurses, therapists, or administrators into suitable roles. We seek to reinforce the architecture behind each hire. Our goal is not to patch holes, but to restore rhythm: matching talent to pressure points with timing, clarity, and clinical relevance.
For decision-makers, we help externalize transformational risk. That means stepping into change without bearing its full cost. Nava brings coordination, structure, and system visibility, so leaders are not building new infrastructure mid-collapse. For internal teams, we reduce operational friction and hiring lag, restoring trust among candidates and managers who have grown accustomed to bottlenecks, ghosting, and delays. And for organizations under financial strain, we help stabilize the cost of staffing by breaking the reactive loop: the endless cycle of vacancy, backfill, and burnout.
We also work to resolve a quieter crisis: the fatigue that sets in when leaders are promised transformation by tools alone. Applicant tracking systems, automated outreach platforms, job boards – none of these are inherently bad but in a system with no underlying alignment, they create more noise than signal. Rather than selling tools, we build the connective tissue that makes those tools useful. Where others automate disconnection, we restore intentional design.
This article marks the hinge in our series. The first four pieces dissected how healthcare hiring fails, not because of bad recruiters, but because of misaligned systems, sluggish tools, and reactive models that were never built to scale.
What follows is not just critique. It is reconstruction.
We begin with the one element every executive depends on, yet few recruitment models actually earn: trust. Not the soft kind. The structural kind. The kind built from transparency, alignment, and accountability at every stage of the hiring funnel.
Nava Healthcare stands beside that redesign. Not with resumes but with infrastructure. With systems that restore traction, partnerships that build trust, and execution support that holds under pressure.
In the next article, we tackle why trust is breaking down between healthcare providers and their recruiting partners, and what it takes to rebuild a model that can actually last.